Top 5 Food Additives Linked to Breast Cancer

Top 5 Food Additives Linked to Breast Cancer Introduction:In the pursuit of a healthy lifestyle, understanding the potential risks associated with everyday choices is crucial. One area of concern gaining attention is the relationship between certain food additives and breast cancer. Dr. Preethi Mrinalini, the chief consultant in Chennai, sheds light on this important topic, […]
Explore the Role of 3D Printing in Breast Reconstruction
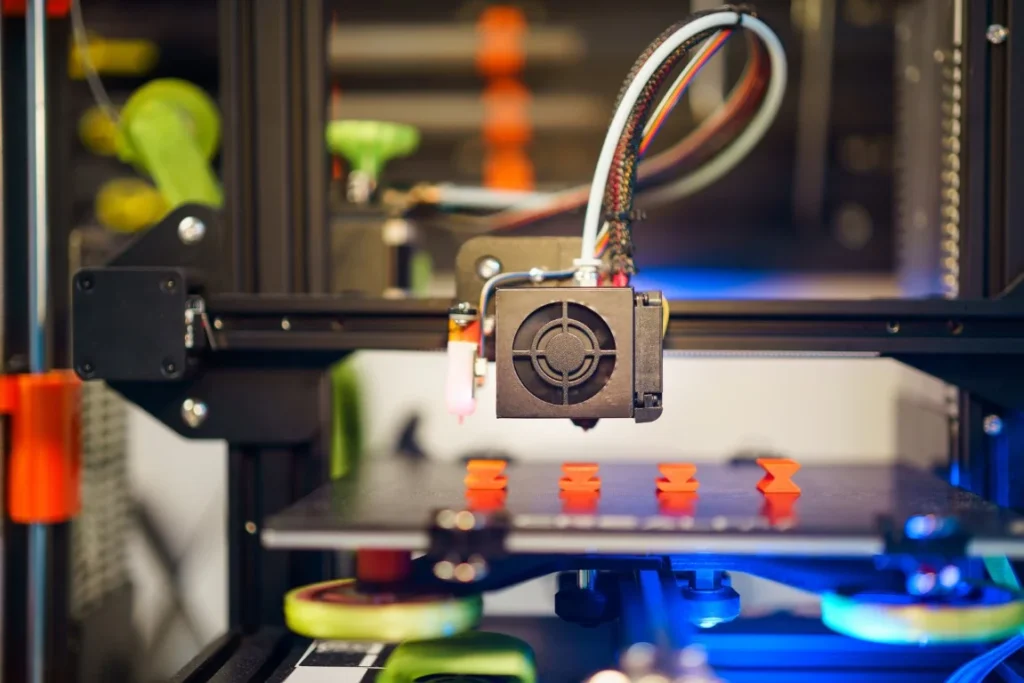
Explore the Role of 3D Printing in Breast Reconstruction Introduction:Facing a breast cancer diagnosis is an overwhelming journey, laden with emotional turbulence and life-altering decisions. Amid the uncertainty, patients often find themselves at a crossroads, contemplating the best course of action for their treatment and, crucially, the journey of reconstruction post-mastectomy. Breast cancer doesn’t merely […]
Robotic Surgery: Gynaecology

Robotic Surgery: Gynaecology A Robotic Symphony in Gynaecology: In the age of advancement where technology and humankind meet, we explore the complex field of robotic surgery, a revolutionary development changing the face of gynaecological treatments. At the core of this investigation is the remarkable Dr Preethi Mrinalini, known as the best female surgeon in Chennai, […]
Surgery Choices for DCIS or Breast Cancer

Surgery Choices for DCIS or Breast Cancer Introduction:Facing a diagnosis of Ductal Carcinoma In Situ (DCIS) or breast cancer can be an overwhelming experience, but understanding your surgery options is a crucial step toward informed decision-making. In this guide, we will explore various surgical choices available, drawing insights from the expertise of Dr. Preethi Mrinalini, […]
Hemorrhoid Treatments: Home Remedies, OTC Medicine, and More

Hemorrhoid Treatments: Home Remedies, OTC Medicine, and More Introduction:Hemorrhoids, often a discomforting and inconvenient condition, affect a significant portion of the population. If you’re dealing with the symptoms of haemorrhoids, you’re not alone. Fortunately, there are various treatment options available, ranging from home remedies to over-the-counter (OTC) medicines. In this comprehensive guide, we’ll explore these […]
What happens if a fissure is not treated?

What happens if a fissure is not treated? When it comes to managing our health, understanding the implications of untreated conditions is crucial. At Marina’s Clinic, we often encounter patients with concerns about fissures, small tears in the skin of the anus that can cause significant discomfort. While fissures may seem minor, their impact on […]
Black Coffee for Weight Loss on an Empty Stomach? | Expert Insights with Dr. Preethi Mrinalini

Why you should include fermented foods in your Diet? Health benefits of fermented foods. Introduction:Have you ever wondered about the magical effects of that humble cup of black coffee, especially when it comes to shedding those stubborn pounds? Well, you’re in for a treat because today, we’re delving into the world of weight loss and […]
Superfoods In Your Kitchen

Why you should include fermented foods in your Diet? Health benefits of fermented foods. Introduction:In the pursuit of a healthy lifestyle, our kitchen can be a treasure trove of superfoods that contribute not only to our well-being but also to the vitality of our immune system. One such category of superfoods gaining popularity for their […]
Why you should include fermented foods in your Diet?

Why you should include fermented foods in your Diet? Health benefits of fermented foods. Introduction: One fascinating and increasingly popular aspect of a healthy diet is the inclusion of fermented foods. Dr. Preethi Mrinalini, Chief Consultant in Chennai, sheds light on the myriad health benefits associated with incorporating fermented foods into your daily routine. Let’s […]
14 Holiday Recipes To Try

Celebrating Safely This Holiday Season IntroductionThe holiday season is upon us, and what better way to celebrate than by indulging in some delightful and nutritious recipes curated by none other than Dr. Preethi Mrinalini, the best female doctor in Chennai. As we embark on a culinary journey, let’s explore 14 mouthwatering holiday recipes that not […]
