Complications of diabetes that affect the feet are caused due to nerve damage – neuropathy, and poor blood circulation – peripheral arterial disease, as a result of long-term high blood sugar levels. Proper blood sugar control is fundamental for diabetic foot ulcer healing. The surgeon first examines the feet for any signs of infection, ulcers, calluses, or other abnormalities. Tests will be performed to assess nerve function, blood circulation, the extent of any existing wounds and the presence of bacteria in order to provide antibiotic treatment if needed. Our surgeon will closely monitor the progress of the infection and approach with personalised diabetes care plans. The treatment will help facilitate faster healing and reduce the risk of further complications by redistributing weight away from the ulcer site.
Patients will be instructed to follow a strict diabetes management plan, which includes proper diet, regular exercise, and adherence to prescribed medications. By combining our surgeon’s expertise, advanced treatment modalities, and patient-centred approach, we aim to promote optimal healing outcomes, prevent complications, and improve our patients’ overall health.
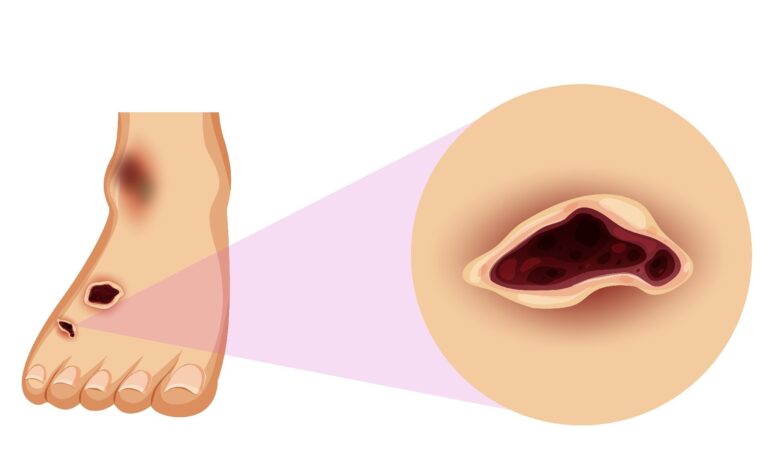
Drainage from your foot, which can stain your socks or leak out in your shoe, is one of the first symptoms of a foot ulcer. Early signs include unusual swelling, irritation, redness, and odours in one or both feet.
The black tissue (called eschar) that surrounds a severe foot ulcer is the most visible symptom. This happens when there isn’t enough healthy blood flow to the region around the ulcer.
Around the ulcer, partial or full gangrene, which refers to tissue death caused by infections, may develop. There may be odorous discharge, discomfort, and numbness in this case.
Foot ulcers do not always show symptoms. Ulcers can often go unnoticed before they become infected.
If you notice any skin discoloration, especially blackened tissue, or if you experience pain around an area that appears calloused or irritated, consult your doctor.
The Wagner Ulcer Classification System will most likely be used by your doctor to determine the severity of your ulcer on a scale of 0 to 5: 0: there are no open lesions; the lesion may have healed.
1. A shallow ulcer that does not reach deeper layers
2 A more serious ulcer that extends to a tendon, bone, or joint capsule
3. Abscess, osteomyelitis, or tendonitis affect deeper tissues.
4. Gangrene in a forefoot or heel section
5. A gangrenous infection that affects the entire foot
Stay off your feet to avoid ulcer pain. This is known as off-loading, and it is beneficial for all types of diabetic foot ulcers. Walking can aggravate an infection and cause an ulcer to swell.
Diabetes-specific footwear includes casts, foot braces, compression wraps, and shoe inserts to prevent corns and calluses.
Foot ulcers can be treated by doctors with debridement, which is the removal of dead skin or foreign objects that may have caused the ulcer.
An infection is a serious complication of a foot ulcer that must be treated right away. All infections are not treated in the same way.
Tissue from the ulcer’s surrounding area may be sent to a lab to determine which antibiotic will be effective. If your doctor suspects a serious infection, an X-ray may be ordered to check for signs of bone infection
One of Chennai’s best gastrointestinal clinics. We provide the most effective treatment for Gastrointestinal Tract, Gallbladder, Stomach, Colon, Rectum, Piles, fissures, and hernias.

© 2024 Marinas Clinic All rights reserved.Powered by Zero Gravity Technologies.